Healthcare payers and providers
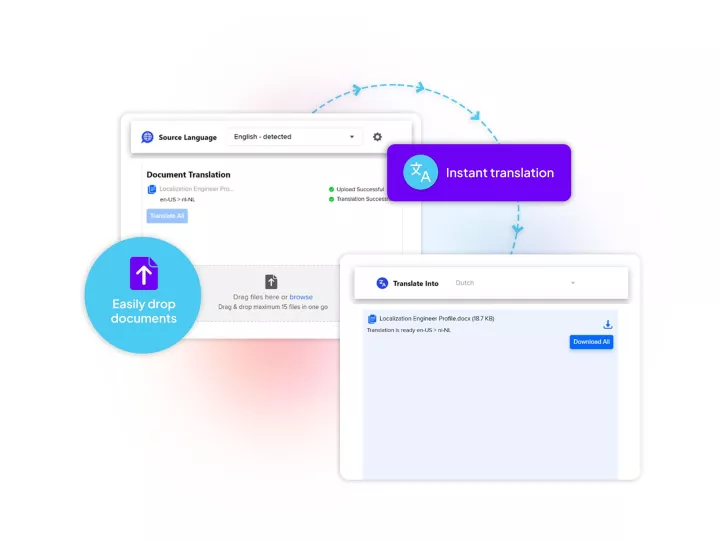
in their language
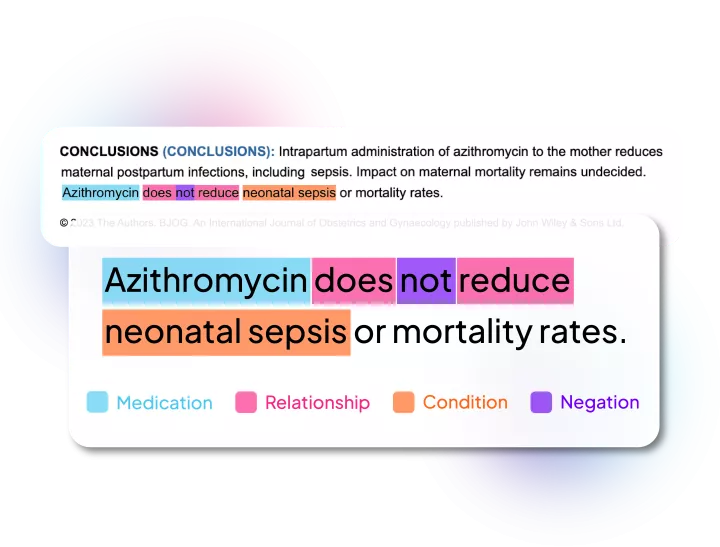
Healthcare NLP and language solutions to improve member care and reduce member risks
From population health analytics to risk adjustment, quality measures, to overcoming accessibility and language barriers